Being told you need a root canal can feel unsettling, but modern endodontic care is far more comfortable and predictable than many people expect. In most cases, a root canal relieves persistent tooth pain, removes infection, and preserves the strength and appearance of your natural tooth — allowing you to keep the tooth rather than having it removed.
At the office of Tiger Family Dental, we combine up-to-date techniques with a patient-centered approach to make treatment efficient and as comfortable as possible. Our team prioritizes clear explanations, careful technique, and measures to minimize discomfort so you can move forward with confidence in your oral health.
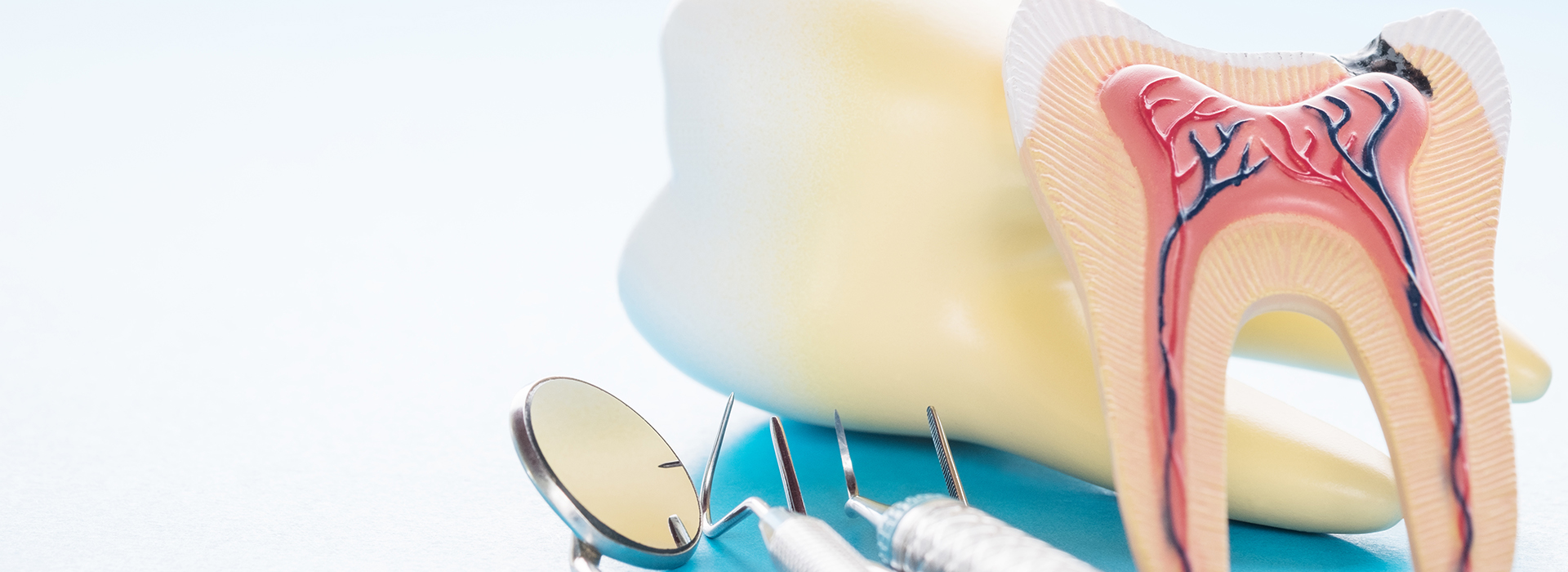
Inside every tooth is a small central chamber that contains the dental pulp — nerves, blood vessels, and connective tissue that support tooth development. When that tissue becomes inflamed or infected, it can cause intense pain and lead to damage that threatens the tooth’s long-term survival. Root canal therapy removes the damaged tissue, disinfects the canal space, and seals it to prevent reinfection.
Removing the diseased pulp does not make the tooth weak in the long term; rather, it removes the source of pain and infection while preserving the natural tooth structure. Once treated, most teeth are restored with a protective restoration such as a crown to restore strength and function and to protect the remaining tooth from fracture.
Root canal therapy focuses on resolving infection and preventing the spread of bacteria to surrounding tissues. This approach helps patients avoid more invasive procedures later and supports the overall health of the mouth and jaw. With proper care after treatment, a tooth that has had a root canal can remain functional for many years, often for life.

Decay, cracks, or trauma can allow bacteria to reach the inner portions of a tooth. When that happens, the pulp responds with inflammation and may become infected. Initially, this process may cause sharp sensitivity to temperature or pressure; if left untreated, it can progress to persistent pain, swelling, and damage to the supporting bone.
Some teeth with pulp damage are obvious because the pain is severe and unrelenting. Others can be more subtle — a tooth may darken, become sensitive only occasionally, or show signs of infection on an X-ray before symptoms are noticed. That’s why routine exams and diagnostic imaging are important for identifying problems early, even when pain isn’t present.
Understanding the cause and extent of pulp damage helps your dentist determine the best route of care. When the pulp cannot recover, root canal therapy is the predictable option that removes the infection and preserves what remains of the natural tooth, helping maintain chewing function and the alignment of surrounding teeth.
Not every toothache requires a root canal, but several consistent signs suggest that the pulp may be compromised. If you notice persistent or worsening symptoms, schedule an evaluation so a dental professional can assess whether root canal therapy or another treatment is needed.
Below are common indicators that a tooth may need root canal treatment. Each item provides a cue to seek care; timely diagnosis improves the likelihood of saving the tooth and limits the risk of more serious infection.
Pain that lingers or returns frequently — especially pain that wakes you at night — can point to inflamed or infected pulp. While causes vary, persistent tooth pain is often a sign that professional evaluation is necessary.
Brief sensitivity is common, but prolonged discomfort when exposed to temperature changes may indicate deeper involvement of the nerve tissue inside the tooth.
Pain when biting down or when the tooth is touched can suggest inflammation or infection affecting the tooth’s internal structures or surrounding tissues.
A tooth that darkens over time can be a sign that internal tissues have been damaged, often from prior trauma or chronic infection.
Structural damage to a tooth can expose the pulp or create pathways for bacteria to enter, making root canal therapy necessary to preserve the tooth.
Swelling of the gums or the appearance of a draining sore often indicates an abscess or localized infection that requires prompt attention to prevent spread.
Infection can compromise the bone and ligaments that hold a tooth in place. In many cases, treating the infection with root canal therapy allows the supporting tissues to heal and the tooth to stabilize.

Delaying care after signs of pulp involvement allows bacteria to proliferate and the infection to deepen, which can lead to more extensive damage to the tooth and surrounding bone. Early treatment limits the spread of infection and often makes the procedure simpler and more predictable.
A tooth that receives prompt root canal therapy is more likely to be restored successfully and to remain functional over the long term. Conversely, neglecting symptoms can result in the need for more invasive procedures or, in some cases, tooth removal when the damage becomes too extensive.
Routine dental exams and X-rays help catch issues before they become urgent. If your dentist identifies a problem that could benefit from root canal therapy, acting without unnecessary delay is the best way to protect your oral health and avoid complications.
Root canal therapy today uses precise instruments and proven techniques to remove diseased tissue, clean and shape the canal system, and fill it with a stable, biocompatible material. Most procedures are performed with a local anesthetic so patients experience little to no pain during treatment. For those with dental anxiety, sedation options can help create a calm, comfortable environment.
The number of visits needed varies by case. Some teeth are treated in a single appointment; others require two or more visits depending on infection control, the complexity of the canal anatomy, and the need for interim medications. Your dentist will explain the plan and what to expect at each stage so you feel informed and prepared.
After the procedure, mild soreness or sensitivity for a few days is common as the surrounding tissues recover. Over-the-counter pain relievers are often sufficient, and we provide guidance on care, eating, and oral hygiene to support healing. It’s important to have the tooth permanently restored — frequently with a crown — to protect the treated tooth from fracture and to restore full chewing function.

At the office of Tiger Family Dental, patient comfort and clear communication are central to our approach. If you have questions before or after treatment, or if you notice persistent symptoms that concern you, please reach out so we can assess your situation and recommend the right steps.
With careful diagnosis, timely care, and an appropriate final restoration, root canal therapy is a reliable way to relieve pain, resolve infection, and preserve your natural tooth. Many patients go on to enjoy full function and health for years after treatment when they follow recommended follow-up care.
If you would like more information about root canal therapy or want to discuss whether this treatment is appropriate for you, contact us to arrange an evaluation. Our team can explain the process, answer your questions, and help you make an informed decision about your oral health.

A root canal is a dental procedure that removes inflamed or infected pulp from inside a tooth, disinfects the canal system, and seals it to prevent reinfection. This therapy preserves the natural tooth structure and restores function when the pulp cannot recover on its own. It is a predictable, tooth‑preserving alternative to extraction when the nerve tissue is irreversibly damaged.
Root canal treatment is typically necessary after deep decay, a fracture that exposes the pulp, or trauma that compromises the tooth’s internal tissues. Persistent symptoms such as ongoing pain, swelling, or a tooth that has darkened are common reasons to consider treatment. Early evaluation improves the likelihood of saving the tooth and avoiding more extensive procedures.
The source of sharp or lingering tooth pain is often the inflamed pulp inside the tooth; removing that tissue eliminates the source of pain and reduces the risk of spreading infection. During treatment the dentist cleans and shapes the root canals, disinfects the spaces, and fills them with a stable, biocompatible material to seal out bacteria. Sealing the canal system stabilizes the tooth and prevents recurrent infection that would otherwise damage surrounding bone and tissues.
Preserving the natural tooth maintains chewing efficiency and helps keep adjacent teeth in proper position, which supports long‑term oral health. After the canal system is treated, placing an appropriate restoration such as a crown restores strength and reduces the risk of fracture. With timely care and a proper final restoration, many treated teeth remain functional for many years.
Several consistent signs suggest the dental pulp may be compromised, including constant or recurring pain, prolonged sensitivity to hot or cold, and pain when biting or touching the tooth. Other warning signs include a tooth that darkens in color, visible chips or cracks, swelling of the gums, or a draining sore near the tooth. Any of these symptoms merit prompt evaluation because early diagnosis increases the likelihood of saving the tooth.
Not every toothache requires a root canal, but subtle or intermittent symptoms can still indicate internal damage that appears on X‑rays before you feel severe pain. Routine dental exams and diagnostic imaging help catch problems early, even when discomfort is minimal. If your dentist identifies pulp involvement, they will explain whether root canal therapy or another approach is the best option.
Diagnosis begins with a clinical examination that assesses symptoms, visual signs of damage, and response to tests such as percussion and thermal sensitivity. Dentists use radiographs and, when needed, three‑dimensional imaging to evaluate the extent of infection, bone involvement, and canal anatomy. These diagnostic tools help determine whether the pulp is inflamed, infected, or capable of healing without root canal therapy.
In some cases, the dentist may place the tooth under local anesthetic to perform additional tests or refer to an endodontist for complex anatomy or persistent symptoms. A clear diagnostic plan ensures you understand the rationale for treatment and the expected outcome. Timely identification and treatment planning reduce risks and improve long‑term prognosis.
Root canal therapy is usually performed under local anesthesia to ensure comfort and begins with isolating the tooth using a rubber dam to keep the area dry and free of saliva. The dentist creates a small access opening, removes the diseased pulp, and uses specialized instruments and irrigation to clean and disinfect the canal system. Once the canals are shaped and disinfected, they are filled with a biocompatible material and the access is sealed with a temporary or permanent restoration.
The number of appointments depends on infection severity and canal complexity; some teeth are completed in a single visit while others require an interim medication and follow‑up. Your dentist will explain the expected treatment timeline, signs to monitor during healing, and the recommended schedule for placing a final protective restoration. Clear communication about each step helps you feel prepared and informed throughout the process.
Most patients experience little to no pain during the procedure because local anesthesia numbs the area and modern techniques minimize discomfort. For patients with dental anxiety or complex cases, sedation options can create a calm and controlled environment so treatment proceeds smoothly and comfortably. Our approach focuses on effective pain control and gentle technique throughout the appointment.
After the procedure, mild soreness or sensitivity for a few days is common as tissues heal, and this is typically managed with over‑the‑counter pain relievers and simple home care. If pain increases, swelling develops, or unusual symptoms occur, contact your dental provider promptly for evaluation. Most post‑treatment discomfort resolves quickly and does not interfere with daily activities.
Recovery after root canal therapy is generally brief; many patients return to normal activities the same day with only minor soreness for a few days. You may be advised to avoid chewing on the treated tooth until a permanent restoration is in place to reduce the risk of fracture. Maintaining good oral hygiene and following any post‑operative instructions supports healing and reduces the chance of complications.
Follow‑up visits allow the dentist to confirm healing and to place or adjust the final restoration as needed, and some signs of internal healing continue for weeks to months as bone regenerates. Long‑term success depends on the quality of the root canal filling and the protective restoration placed afterward. If symptoms persist or recur, prompt evaluation helps identify residual issues that can be treated early.
Many teeth treated with root canal therapy benefit from a protective restoration such as a crown because removing pulp tissue can leave the tooth more prone to fracture under chewing forces. A crown or onlay restores strength, protects remaining tooth structure, and helps prevent future damage. Your dentist will assess the amount of natural tooth left and recommend the restoration that best preserves long‑term function.
In some cases, a well‑filled canal and adequate remaining tooth structure allow for a direct composite restoration rather than a crown, particularly on front teeth with lower bite forces. Whatever the chosen restoration, timely placement is important to protect the treated tooth and maintain occlusion and chewing efficiency. Regular monitoring at dental checkups ensures the restoration remains secure and functional.
Root canal therapy targets the source of infection inside the tooth, removing bacteria and inflamed tissue so the surrounding bone and soft tissues can heal. By eliminating the reservoir of infection, the procedure reduces the risk of abscess formation and further bone loss that could compromise adjacent teeth. Controlling localized infection also helps maintain stable bite relationships and chewing function.
While a root canal addresses the infected tooth itself, comprehensive oral care—including routine exams, professional cleanings, and prompt treatment of new decay—helps protect overall oral health. In cases where systemic antibiotics are appropriate, your dentist will prescribe them; however, the definitive resolution of infection usually requires removal of the diseased pulp and proper restoration. Ongoing follow‑up ensures the treatment remains successful.
At the office of Tiger Family Dental we prioritize patient comfort through clear communication, modern technology, and individualized sedation or anesthetic options when needed. Our team explains each step of treatment, answers questions up front, and uses techniques that minimize discomfort and shorten chair time. Creating a relaxed, supportive environment helps patients feel confident about moving forward with necessary care.
In our Sedalia office we combine digital imaging and gentle operative protocols to make diagnosis and treatment more predictable and comfortable. We encourage patients to discuss anxieties or special needs so we can tailor the visit, and we provide practical aftercare guidance to support recovery. This patient‑centered approach aims to make endodontic care as efficient, reassuring, and effective as possible.

Looking to schedule your next dental visit or learn more about our services?
Getting in touch with Tiger Family Dental is simple! Our friendly team is ready to help you book appointments, answer questions about treatments, and address any concerns. Whether you’d like to call, or use our convenient online form, we’re here to assist you. Take the first step toward a healthy, confident smile — contact us today and experience the difference personalized dental care can make.